Being there for Ariel's Cancer
Being there for Ariel's Cancer
Hello! Well, this is not a blog post I expected to write. Let me avoid needlessly worrying you, dear reader, by starting at the end: Ariel had two cancers, it was worse than we thought, but he’s OK and in remission now. This is due to ardent patient advocacy by Ama and me, and the wonderful loving support of our family, friends, and Ariel's sweet caring fans. If you're reading this, you're probably one of them, so thank you from the bottom of our hearts.
Content warning: cancer, surgery, and general medical terminology. Also robots with knives!
Expecting and the unexpected
This story began not long ago, in mid February, 2021. 'Twas the week before a major work project launch. My wife Becka and I were ~10 weeks away from having our 2nd baby, and 3 months into our move up the coast to Byron Shire to be closer to Ama and Ariel; my parents. That turned out to be quite important. Thank you to my employer for supporting remote work!
Ama had some intuition that something was up with Ariel: he had very occasional shortness of breath and acute but short-lived chest pain. So she had been making sure he got a full heart check, just in case.
Her intuition was close enough: a chest x-ray revealed a mass in Ariel’s chest near his heart; likely a haematoma or lymphoma. They said it was the size of a golf ball, but 6.7cm looked more like a potato to me. He needed to get to a specialist, quickly. Cue the next-day GP appointment for a referral.
First, you wait for more information
Ariel's GP said it would probably be a month until we really knew what was going on, but from what we knew:
“It’s not a death sentence.”
A sentence itself both reassuring and confronting. Enough for its own quote, bold, and italics.
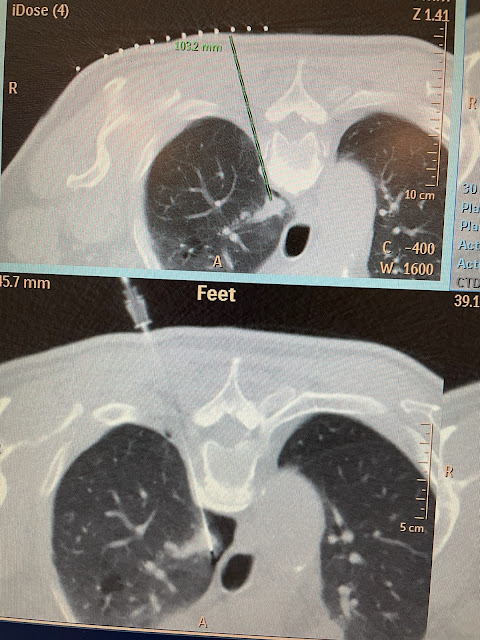
In fact, it was almost a month until just the biopsy in mid March, as there was a complication: a PET CT scan revealed a nodule of cell “activity” in Ariel’s lung. That meant either cancer or a very localised infection, and the latter was rather unlikely. Unfortunately, the lung nodule was close to a notable vein, so the surgeon thought it too risky to biopsy. Fortunately it seemed very small, so we could focus on figuring out what kind of potato (sure, let’s call it that) was in front of his heart. We hoped it wasn’t lymphoma.
A biopsy doesn’t sound like a major procedure, and if you can get it done with a needle, it isn’t necessarily. But the surgeon wanted to ensure we got enough tissue for the pathology lab, so he made a ~6cm incision between a pair of ribs to get some tissue out. It wasn’t pretty.
A week later, we got the diagnosis: Thymoma, Type B2. The oncologist said it was “low grade” and “slow-growing”, so the surgeon wanted Ariel to heal up before he goes back in to remove it (thymectomy), as well as the lung nodule (wedge resection), as it’s probably lung cancer. So he’ll call us back in a month.
… Wait, what?
Don’t just take what you’re given
Ariel didn’t like that the surgeon barely checked on him and generally didn’t seem on the ball, and I was keen to get a 2nd opinion anyway. My own life insurance has a benefit of free medical 2nd opinions from world experts through http://bestdoctors.com, which applies to direct family. We had previously used it for Ama’s breast cancer a few years back, too.
This all sounds quite calm and clinical when I write it down, and while I certainly had my level head on and we were all supporting each other, there was a serious undercurrent of fear and anxiety. When I called Best Doctors, I had to dial 4 times before I got the number right.
In a nutshell, they confirmed what I had been thinking: Ariel was likely eligible for minimally invasive robotic surgery. This would dramatically improve his recovery time, as they wouldn’t have to open his chest up or cut through his sternum–or even any bone at all.
Even while waiting to have this confirmed, I had been looking for other cardiothoracic surgeons–particularly those who perform robotic thymectomies and wedge resections. It turned out the best place for that was in Sydney, and within 48 hours of my reaching out to one of the top surgeons to see if Ariel was eligible, we had an initial phone consult.
Dr Levi Bassin had reviewed Ariel’s scans, was willing to take him on, and strongly recommended coming in ASAP. Through the simple and affordable wonders of private health insurance, Ama took Ariel down to Sydney and checked him into North Shore Private 12 days later. Surgery would be another 3 days, on the 24th of April. Just under 10 weeks since the x-ray that unearthed that damned potato.
… and 7 days before Becka and my second child was due! Which is why I couldn’t go too.

My father, Ariel, serenely preparing to go under the robotic knife.
Oh, but one more thing: those 3 days before surgery were for many pre-op tests. One of which was a simple needle biopsy of the lung nodule. Because the radiologists in Sydney had the expertise and equipment, and Dr Bassin wanted to know exactly what we were dealing with before he went in.
Within hours, we had it confirmed: lung cancer. Early on (Stage 1A), thankfully, but definitely needed to be removed.
And remove it he did: Dr Bassin gave us the good news that he had been able to remove all the cancer, both thymoma and lung. However… the thymoma was actually highly aggressive: it had begun to invade the lining of the heart and of the lung, a major vein, and the left phrenic nerve. So there was a fair bit of collateral damage, and to fix it required a full sternotomy; effectively open heart surgery.
Finally, the best worst part: if we had waited to have the surgery, it might not have been possible. Another 2 months and it would have been inoperable; quite possibly a death sentence after all.
Recovery can be full of disconnect and pain
Ariel had 5 drainage tubes going through his belly about a foot deep into his chest. Those tubes hurt so much, and there was only so much morphine could do. Walking was difficult even with help, but necessary. Recovery was hard.

That biopsy scar is looking a lot better after the 2nd surgeon reused the incision site!
After a few days, they were able to remove the tubes. And every day, Ariel felt better–with ups and downs. Less than a week after such a major surgery, he was all set to fly home with Ama!
Recovery can be complicated
As Dr Bassin handed back the Medical Clearance to fly, Ama asked him about Ariel’s swollen left arm, which a nurse had said was no issue. The shock on Dr Bassin’s face was followed by a quick order for tests which soon confirmed Ariel had three deep vein thromboses (clots) and could not fly for another week while they filled him with blood thinners.
Again, Ama’s intuition and careful attention saved the day. Shortly after, she had to fly home to rest and recuperate. Caring for someone facing or recovering from life-threatening illness is exhausting, and she needed to take care of herself a bit.
By then, my second son had been born! So while I wanted to be home as much as possible, Becka's capable caring for both our children enabled me to fly to Sydney for two days to be with Ariel and bring him home.

The first place we went from the hospital was a nice park. The second was a Phở restaurant!

The moment Ariel met my newborn son brought tears to my eyes.
Modern medicine deals with many complications
Alas, the story was not quite over. On his first two nights home, Ariel had stabbing chest pain. On day three, Dr Bassin sent him to the local Byron Hospital ER, where the good news was that he did not have a blood clot in his lungs. No, he just had a lot of fluid.
Off they passed him to a Gold Coast hospital, where they were equipped to insert another one of those painful drainage tubes. Thankfully he had the foresight to pack and bring an overnight bag. They drained over 750ml of fluid before finally sending him home after three days–last Thursday.
The next steps will be radiotherapy to ensure that aggressive thymoma does not come back.
The future is bright, when we help each other
In the meantime, he’s continuing to recover, day by day, bit by bit. But he’s definitely on his way back, and it’s an absolute joy to see both my parents relaxing again as our family bonds run deeper. There are few greater opportunities to deepen love as in supporting each other through crises. And that goes not only for family, but everyone who helped us shoulder some of the burden along the way: thank you again for being there for us.






I finished reading, Joel, you're a gem ! Thanks for this clear report which makes more palpable for me to realize what Ariel went through ! My Goddess..... Amazing. How much love and care make a difference..Bravo for this clear and touching report .... Margot
ReplyDeletemerci pour ce récit très touchant.
ReplyDeleteIs good to hear Ariel is doing well , regards to Alma and Ariel! Take care.
ReplyDelete